The Case
I was in the rural surgery clinic seeing patients when the ED physician called the general surgery phone frantic that a 6-month-old child is choking in the ED. The mother can be heard screaming in the background “please don’t let me baby die.” The ED physician states the baby swallowed a watch battery, and I immediately leave the clinic, called the OR and requested the GI team meet me in the ED.
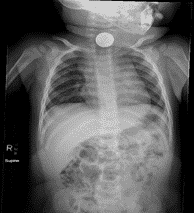
Upon arriving in ED, I evaluated the child, reviewed the images and quickly discussed the options with the ED provider, the anesthesia provider, and EMS. With the location of the foreign body in the infant’s esophagus, it would have not been safe to transport him to another facility with a pediatric provider.
In the ED, after consent was obtained, I performed an emergent EGD and removed the foreign body. The entire procedure took less than 3 minutes.

Upon completion of the procedure, I spoke with family and noticed that the entire ED waiting room, hallways, and even the parking lot was completely filled with concerned community members – who were relieved that this critical access hospital could fulfill it’s mission statement of providing emergency surgical care to it citizens.
This critical access hospital – situated in a county with a population of 6000 – had decided 3 months prior to start a fulltime surgicalist program. The program was growing but the community was either not completely aware of the program or unconvinced of our skillset. Following the reports of this emergent procedure, the outpatient clinic visits increased by 42% in the next 3 weeks. In addition, the number of commercially insured ER visits increased by 52% over the next month.
The Problem
Rural hospitals have the enormous responsibility of providing high quality emergency care to their citizens. With decreasing reimbursements and difficulty developing / maintaining specialty service lines, these rural facilities have the difficult responsibility of trying to fulfill mission statement to their community. In particular, the ability to maintain a full-time general surgery program is a daunting task. The shortage of general surgeons is well documented throughout the United States – but the shortage of these specialist in the rural community is more than a press release – it is an unfortunate reality.
According to an April 2019 report by the AAMC, there is a critical shortage of general surgeons that is only expected to increase over the next decade. By 2032, the shortage of general surgeons is expected to exceed 23,000. As the number of the classic rural general surgeon continues to decrease with retirement and burnout along the increasing trend of >90% of all graduates seeking specialty fellowship training, the pool of general surgeons to provide services to rural communities will continue to decrease.
According to Merritt, Hawkins & Associates, the overall cost (including lost revenue) of recruiting a general surgeon exceeds 1.5 million annually. This cost includes salaries, recruitment fees, interviewing, relocation, practice marketing, and lost revenue (while searching for the surgeon).
The recruitment and retention of general surgeons is often the limiting factor in not only building a successful general surgery program – but maintaining it. The need for a highly skilled surgeon often leads facilities to offer lucrative, multi-year contracts in the hope that the right surgeon is selected. Whether it is time commitment, burn out or family pressure, often the grand opening of the surgery clinic is quickly replaced with a new general surgeon search. In addition to the lost revenue and possible protracted legal battle of an unexpected surgeon departure, the new devices, materials, and community disappointment add to the significant financial burden the facility is faced with.
Unfortunately, many rural facilities are forced to explore short-term fixes to this long-term dilemma. Locums tenens and other temporary solutions fail to provide the facility or community with the continuity of care required to develop long term trust – and the unsustainable cycle continues.
The Solution
For rural and critical access hospitals, the daunting task of building a successful surgery program is well documented. Over the last decade, the “surgicalist” has become a possible solution to address these concerns. Unlike their urban center counterparts, these rural surgicalist are responsible for both inpatient and outpatient surgical care – which allows the facility to address emergency surgery care and build a robust elective practice – which in turn increases the facility’s market share of commercially insured patients.
Currently, there are industry leaders building full-time and custom part-time general turnkey surgery program that addresses the clinical needs of your community and the financial concerns of the hospital.
These programs virtually eliminate the concern of long-term contracts, unproductive surgeons, and unrecoverable expenses. The companies that offer these services recruits highly skilled, board certified general surgeons that are dedicated to bringing gold standard surgical care to rural communities.
But be careful – in choosing to partner with a surgicalist company, each facility must ensure that the company is committed to working collaboratively with your key stakeholders to build the key elements of a complete surgery program – including the outpatient clinic. They must understand that with the development and expansion of the elective practice – your facility will increase its market share of commercially insured patients – therefore increasing your facility’s bottom line. Finally, the firm must comprehend that targeted marketing and outreach will make your general surgery program a desired surgery location for not only your local community but regionally. If any of these are missing, keep searching.
The principles for building a successful Rural Surgicalist program are the following:
- An administration that recognizes the NEED for a surgery program
- A community and primary care providers that WANTS a surgery program
If you answer YES to #1 & #2, a rural surgicalist program may be the answer to your surgery problem.
G McClain, MD




